About Us
The Mesoamerica Health Initiative / Salud Mesoamerica Initiative (SMI) aims to reduce maternal, neonatal and child health (MNCH) inequalities through a results-based financing (RBF) model. At the beginning of the Initiative, among the poor in Mesoamerica, only 5 out of every 10 births were attended by skilled health personnel. The mortality rate among newborns and children under 5 was twice the regional average. And children from the poorest 20% were 6 cm shorter than those from the richest 20%.
SMI has been implemented by the Inter-American Development Bank (IDB) in three operations:
- The First Operation focused on “system readiness” by improving inputs, norms, guidelines, and organization of the health networks.
- The Second Operation focused on increasing coverage and improving quality; and
- The Third Operation focused primarily on quality and impact indicators, like anemia prevalence.
Our Results-Based Financing (RBF) Model
Our Results-Based Financing (RBF) Model SMI implements a results-based financing (RBF) model, which makes both donors and aid-recipient countries rethink the traditional approach to financing and emphasizes achieving results. There is enough evidence in public health for what works, but not necessarily how solutions should be implemented, especially in hard-to-reach areas.
The Initiative’s theory of change establishes that the combination of financial and reputational incentives, evidence from external performance monitoring, and additional resources allocated to the poor would motivate the adoption of evidence-based interventions and policies that increase demand and supply of health services. In some cases, this means testing “operational innovations” to bring biomedical interventions to target populations. In turn, this supply-and-demand cycle would improve health among the poorest populations in Mesoamerica.
The SMI model is based on four basic concepts:
1) Countries must focus on the poorest 20% of their populations, selected based on Poverty Incidence Data;
2) SMI funds can only finance evidence-based, cost-effective, and promissory interventions for maternal and child health;
3) All projects are co-financed by SMI and countries (50-50 cost-sharing); and
4) 4) All results are externally and independently verified by the Institute for Health Metrics and Evaluation (IHME) of the University of Washington, through both household and health facility surveys. If countries meet 80% of their goals, they receive 50% of their original investment to use freely for health projects.
In the region, SMI interventions directly benefitted 1.8 million women of reproductive age and children less than 5 years of age, as well as 4.5 million people living in the poorest areas indirectly.
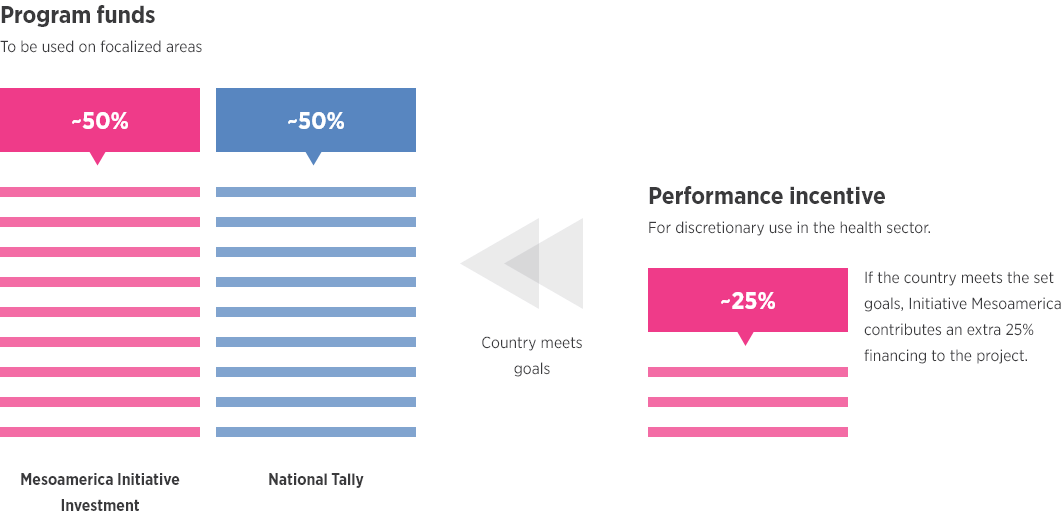
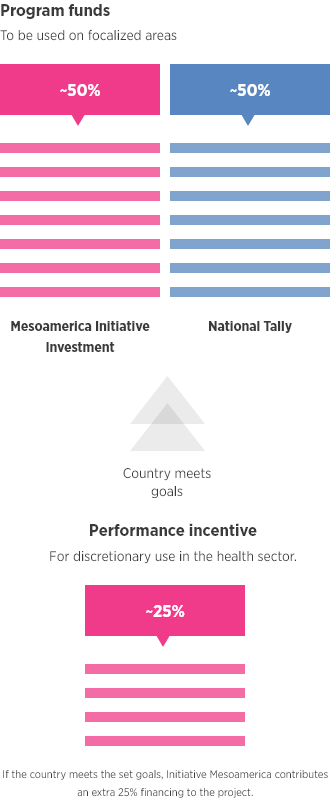
At the start of SMI, each country received an investment donation that was matched by country domestic funding to implement evidence-based interventions in the poorest areas. If the country met the previously agreed targets, it received an incentive (the performance tranche) that reimbursed half of the country’s funds initially invested for unrestricted use within the health sector.
SMI’s RBF model considers different measures to mitigate the risk for perverse incentives and prevent beneficiaries from focusing on some indicators only: a minimum score of 0.8 must be obtained for the disbursement of the performance tranche (PT). Results indicators and life-cycle approaches ensure that the program keeps focused on improving health. An evaluation in comparison areas is performed to ensure funds are not transferred from some areas to others.




